How Sleep May Be Affecting Your Chronic Pain

Posted November 27, 2023
Common Causes Of Chronic Pain
Pain is part of the normal human experience. The brain is designed to assess any potential threat to our body and will use pain as a means to protect. By definition, chronic pain is pain that has lasted beyond the expected healing time. This timeline is dependent on the type or nature of injury with most healing timeframes between 4-12 weeks. Acute pain can be accompanied by inflammation, soreness, stiffness, and difficulty using the injured area in daily tasks, which are all part of the body’s natural healing process.
These processes are designed to promote tissue healing and keep our bodies “safe”. With chronic pain, although the tissues have healed, the body’s nervous system or “alarm” system stays “on alert” even though the tissues have healed and the “threat” to our health and safety is resolved. This extra sensitive alarm system can allow pain to persist and make participating in normal daily activities difficult. Other causes of persistent pain can include degenerative diseases, Fibromyalgia, inflammatory arthritis, and cancer, among others.
Extensive research on chronic pain has shown us that several factors can contribute to the persistence of pain after the tissues themselves have healed. These involve things you wouldn’t expect – like fear or anxiety about the pain, avoidance of physical activities, financial and family stress, poor sleep, and socioeconomic status. Any of the above can keep your system extra sensitive, ultimately amplifying and prolonging your pain experience.
The good news is there are many ways to dial down our system to make it less sensitive and lower the perceived threat for our brain. One crucial part of this process is getting regular, restorative sleep. A good night’s sleep, combined with good nutrition and exercise, can assist in the natural healing processes of our bodies.
Benefits Of Getting A Good Night’s Sleep
We all know that sleep is an essential function in maintaining our physical and mental wellbeing, however, most will experience some level of sleep disturbance at some point in our lives. This can be frustrating for many, but typically those periods are episodic and short lived.
For those with persistent pain, sleep disturbances can amplify and prolong the pain experience. In fact, lack of sleep can even sensitize the system of those without preexisting pain! Getting your sleep back on track is one of the most important steps toward recovery in the treatment of chronic pain. Poor sleep can even increase the likelihood of future chronic pain issues.
Sleep is an essential part of human existence because it is the primary healing time for our brains and bodies. Although everyone’s needs differ, we should strive for around eight hours per night of deep, restful sleep.
Sleep is also important for:
- Neural maturation
- Assisting with learning or memory
- “Cleaning up” or eliminating unimportant neural connections that might clutter the overall network
- Clearance of waste products generated by activity in the awake brain
Our Sleep Cycle Includes The Following Stages:
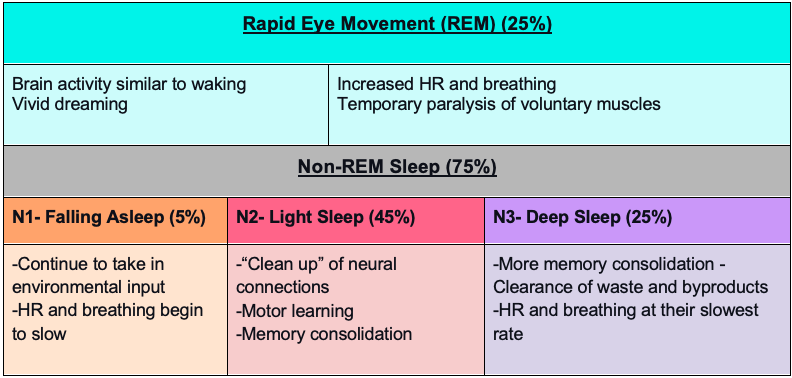
It’s important to note that just because you “slept” for eight hours does not mean it was restorative quality sleep. Many people do not achieve adequate deep sleep, meaning although they lay there for eight hours, their bodies and brain don’t repair fully overnight. It is crucial to prioritize and work on sleep hygiene (the routine and habits around sleep) to achieve adequate rest for healing.
Your Therapist’s Role in Sleep Health
Your therapist knows the importance of sleep in physical, emotional, and psychological healing, especially regarding chronic pain. Your PT or OT will inquire about how you are sleeping, your bedtime routine, your habits in the afternoon and evening, your exercise routine, your stress levels, and your diet to gain an idea of your sleep quality. Here are some suggestions your therapist may make to help you regain restorative sleep while improving your ability to participate in daily activities:
- Go to bed at a regular time and practice a “no device” policy 2 hours before bed.
- Humans work on a 24-hour circadian rhythm and are sensitive to light, especially from phones, computers and TVs. If we practice going to bed at the same time every night and limit light, we will sleep more deeply.
- Get adequate exercise.
- Physical movement is one of the best ways to achieve restful sleep, as our bodies produce hormones that signify the need for rest after exercise.
- Limit alcohol and caffeine before bed.
- You may think that alcohol helps sleep, but research shows that sleep is much lighter when there is alcohol in your system. Caffeine has a half-life of around six hours, meaning if you drink coffee at 2:00 pm, half is still in your system at 9:00 pm! For the best sleep, caffeine shouldn’t be consumed past noon.
These are only a few of many strategies that your therapist might recommend to help your sleep and, ultimately, your chronic pain. Your therapist may also refer you out to a sleep specialist if sleep apnea is suspected. When we sleep well, we have the foundation for mental and physical healing and living life to its fullest!
Supporting Evidence
- Patel AK, Reddy V, Shumway KR, et al. Physiology, Sleep Stages. [Updated 2022 Sep 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526132/
- Roehrs et al, 2015 Sleep in America® Poll
- Whale, K., Dennis, J., Wylde, V. et al. The effectiveness of non-pharmacological sleep interventions for people with chronic pain: a systematic review and meta-analysis. BMC Musculoskelet Disord 23, 440 (2022). https://doi.org/10.1186/s12891-022-05318-5
- Finan et al. The association of sleep and pain: an update and a path forward. The Journal of Pain. 2013:14(12). 1539-1552.
- Simpson et al. Chronic exposure to insufficient sleep alters processes of pain habituation and sensitization. Pain. 2018: 159(1). 33-41.











































 Director of Marketing, Training and Professional Development
Director of Marketing, Training and Professional Development Marketing Consultant | Boutique Partners
Marketing Consultant | Boutique Partners Digital Marketing Specialist
Digital Marketing Specialist Digital Marketing Manager
Digital Marketing Manager Senior Graphic Designer
Senior Graphic Designer Content Production Manager
Content Production Manager Graphic Designer
Graphic Designer Senior Director of Partner Growth
Senior Director of Partner Growth Hive Marketing Liaison
Hive Marketing Liaison Digital Marketing Campaign Specialist
Digital Marketing Campaign Specialist Marketing Analyst
Marketing Analyst VP Brand Communications
VP Brand Communications  Web Designer
Web Designer Marketing Communications Specialist
Marketing Communications Specialist PR + Communications Manager
PR + Communications Manager Senior Director, Consumer Media Group
Senior Director, Consumer Media Group